The relationship between diet and mental health is increasingly being recognised as a critical component of our overall wellbeing. This article will explore how a balanced diet may contribute to better mood and emotional resilience. We'll also look at how a poor or restrictive diet can worsen or even trigger mental health conditions. Dive in and learn more about the multifaceted connection between diet and mental health, covering everything from the roles of specific nutrients like protein to the effects of fad diets, gut health, and much more on our mood and wellbeing.
Nutrients for mental health
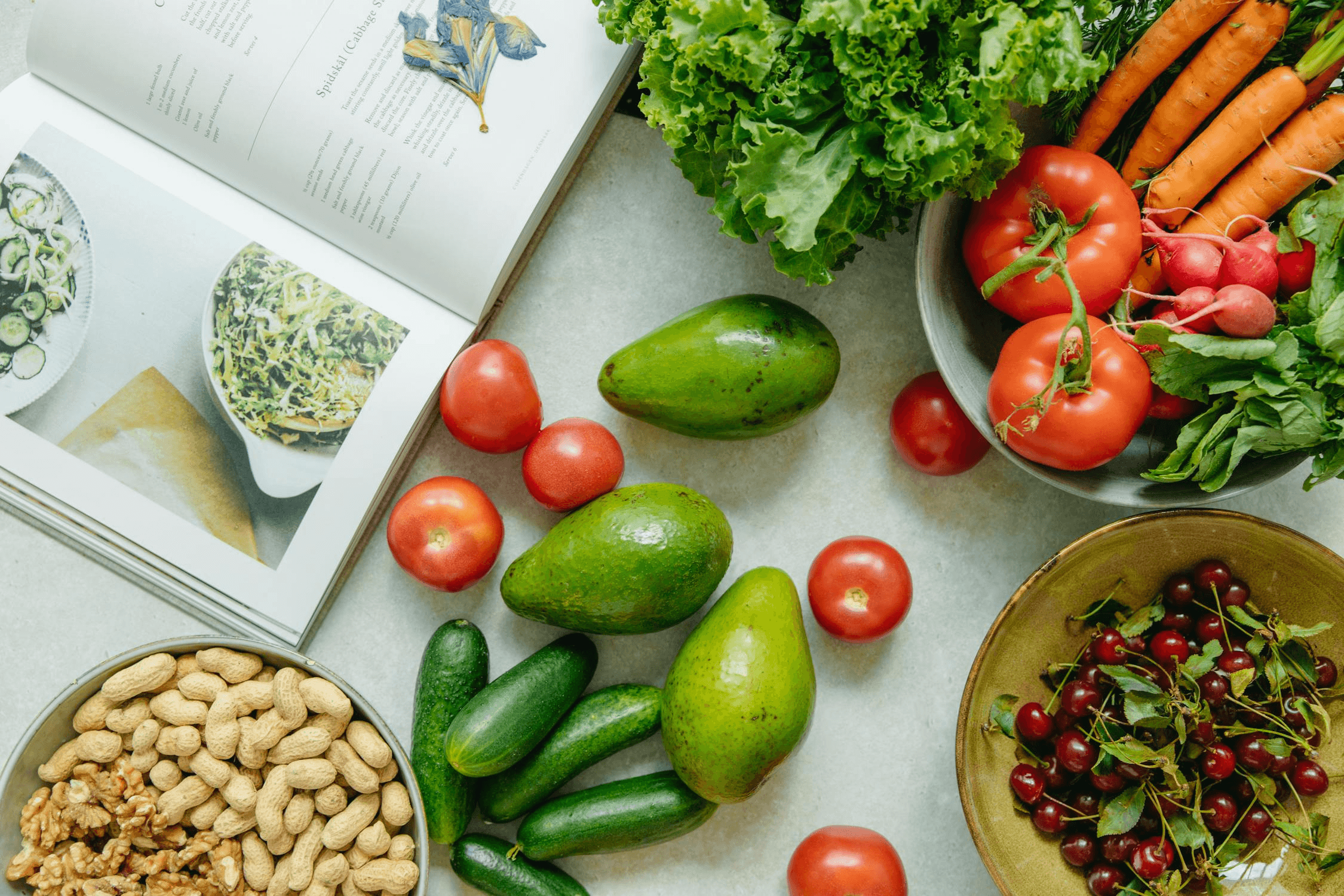
There are numerous nutrients which play their part in making us look and feel our best. However, there are a few key players for mental health. The most common nutritional deficiencies seen in those suffering from mental health disorders are omega-3 fatty acids, B vitamins, minerals, and amino acids that are precursors to neurotransmitter synthesis.[1] Let's look at some of these in more detail to understand more about why they're so important.
Protein and mental health
Protein is a macronutrient and has multiple important roles in the body, including a significant influence on mental health. One of its key functions is providing amino acids that serve as the building blocks for neurotransmitters. These are chemical messengers in the brain that help regulate mood, motivation, and cognitive function. Low levels of these brain chemicals have been associated with mood disturbances, anxiety, and fatigue. One of the most significant is serotonin, often referred to as the "feel-good" chemical, as it plays a vital role in mood regulation, emotional balance, and sleep quality. It is synthesised from the essential amino acid tryptophan, which must be obtained from protein in the diet. Consuming enough protein may help prevent mood disturbances and support stable energy levels [2,3]. Good sources include chicken, turkey, beef, pork, eggs, dairy products, fish, tofu, nuts, beans, seeds, milk, and oats.
Explore more in our blog: Can Protein Help to Support Mental Health?

Blood sugar and mood
Blood sugar instability can significantly affect mental health. Rapid spikes and crashes in blood sugar levels, often caused by consuming high-sugar or refined carbohydrate meals, can lead to symptoms such as irritability, fatigue, and difficulty concentrating. Certain foods can help to keep blood sugar levels more stable:
- Protein - Protein-rich meals can help to stabilise blood glucose levels by slowing the absorption of carbohydrates, which can indirectly support emotional stability and energy levels. By moderating these fluctuations, protein contributes to a more balanced release of energy and helps prevent mood swings linked to glycaemic variability. [4]
- Fibre - Fibre, especially soluble fibre, can help regulate blood sugar by slowing the absorption of sugars into the bloodstream.. This leads to a steadier supply of energy throughout the day, reducing the likelihood of sharp spikes and drops in blood sugar levels. [5] Find out more about the benefits of fibre on our blog. Whole grains, nuts, fruits, and vegetables are good sources of fibre.
Stabilising blood sugar through a combination of protein, fibre, and complex carbohydrates may help to support better mental and metabolic outcomes [6].
B vitamins and mental health
In addition to protein and fibre, other dietary nutrients are known to support mood and mental health. B vitamins, particularly B6, B9 (folate), and B12, are essential for neurotransmitter synthesis, including serotonin. Deficiencies in these nutrients have been linked to depression and cognitive decline [7,8].
Good sources of B vitamins include whole grains, legumes, leafy greens, eggs, dairy products, and meat. However, vitamin B12 is almost exclusively found in animal-based foods, making it especially important for those on plant-based diets to ensure that they obtain B12 through fortified foods or supplements.[9]

Omega-3 fatty acids and mental health
Many people try to avoid fats in their diet, assuming all fats are unhealthy, but not all fats are the same. Certain fats are essential for both mental and physical health. Omega-3 fatty acids, particularly EPA and DHA, are types of healthy fats that are crucial for brain function and emotional balance. They help build brain cell membranes and have anti-inflammatory properties, which is important because inflammation in the body has been linked to depression [10]. Reducing inflammation may be one way omega-3s help to improve mood and mental health.
Since our bodies can't make these fats on their own, we need to get them from food. The best source is oily fish, such as salmon, mackerel, and sardines. For those on a plant-based diet, options like chia seeds, flaxseeds, walnuts, and soybeans offer a form of omega-3 called ALA, which the body can partially convert into EPA and DHA. Low intake of omega-3s is common in Western diets, and this deficiency may increase the risk of depression and other mood disorders. Supplementing with EPA, in particular, has shown positive results in studies looking at treatment for major depression. [11,12].

Gut health and the brain
The gut-brain axis is a complex communication system between the gastrointestinal tract and the brain, and it plays a vital role in mood regulation. The connection between the gut and the brain hinges on the fact that the good bacteria living naturally in our gut play a significant role in the synthesis of neurotransmitters like GABA and serotonin, which have a positive effect on our mood.[13] Additionally, the brain, the gut microbiome, and the immune system are all connected through the vagus nerve, a primary part of the parasympathetic nervous system, which controls mood, as well as inflammatory immune responses and digestion. Our gut bacteria positively affect the activity of the vagus nerve. [14].
Good gut bacteria are increasingly recognised as being very important for good health and wellbeing. An unbalanced gut microbiota, called 'dysbiosis', can be caused by a poor diet high in ultra-processed foods and sugar, as this feeds bad rather than good bacteria. Other factors like the use of antibiotics [15] and steroids [16], smoking [17] can also disrupt the delicate balance of the gut bacteria populations. Consequently,+\ gut dysbiosis has been associated with poor mental health and is thought to be a factor in anxiety and depression [12]. Diets rich in fibre and fermented foods, such as plant-based or Mediterranean diets, support microbial diversity and emotional wellbeing.[18] Good sources of natural probiotic foods to support the microbiome include yoghurt, kimchi, sauerkraut, kombucha, brined pickles, and miso, plus high-fibre foods which help to feed the good bacteria.

Ultra-processed foods and depression
As mentioned in the previous section, high consumption of ultra-processed foods has been shown to disrupt the gut microbiota. A diet high in ultra-processed foods has been associated with a higher risk of anxiety symptoms and other mental disorders. The cause of this is likely to be due to a variety of factors, including inflammation, poor gut health, nutritional deficiencies, and poor sleep quality. These foods often contain artificial additives, low dietary fibre, and poor nutrient density, characteristics that negatively influence gut microbiota and increase systemic inflammation [19]. A growing body of research confirms that a poor diet and mental health often go hand in hand, particularly in Western populations with high ultra-processed food intake.

Dieting and mental health
We've learned that eating a healthy diet can help to support our mood, but with so many different diets out there, how do we know what a healthy diet is? We can't dismiss all of these dieting strategies - low-carb, low-fat, high-carb, high-fat, intermittent fasting etc. - as certainly some people do better when eating fewer carbs, for example, or more fat, more protein, more plant-based foods, etc. or going for longer periods without food. Our individual health and exercise goals will also play a part in determining the best diet for us, and these needs may change according to our differing lifestyles and life stages.
"While every individual's needs are different, a mentally supportive diet will always include stable blood sugar, good-quality protein, fermented foods and fibre for gut health, and the right balance of healthy fats."
— Kerry Beeson BSc (Nutr. Med..), Nutritional Therapist
The Mediterranean diet
Although different diets will suit different people, there are some diets which are consistently associated with better wellbeing. A good example is the Mediterranean diet, a way of eating based on traditional foods from countries around the Mediterranean Sea, rich in vegetables, fruits, whole grains, legumes, nuts, olive oil, and moderate amounts of meat, fish and dairy. There is a strong and positive association between the Mediterranean diet and mental health, with research suggesting that following a Mediterranean diet may significantly reduce the risk of depression [20]. This eating pattern is rich in fruit, vegetables, protein, antioxidants, omega-3 fatty acids, polyphenols, and fibre, all of which support good gut health, combat oxidative stress, and reduce inflammation.

Fad diets and mental health
Health goals will differ from person to person, so when trying out new diets, it's important to realise that the latest trend may not be right for you. Keeping an eye on your calorie intake to make sure it's right for your needs is fine - and remember, sometimes that may mean eating more rather than fewer calories - but overly restrictive eating patterns have been associated with stress and anxiety, as well as nutritional deficiencies.
Evidence suggests that dieting and mental health are closely linked, especially when restrictive diets interfere with social life, self-image, or micronutrient sufficiency [21]. These diets may worsen outcomes for people vulnerable to eating disorders or anxiety. If you have specific health goals and want to try adapting your diet to support these, it's best to do so with the advice and support of your doctor and a qualified nutrition professional.
Conclusion
We've learned that the link between diet and mental health is not only real but increasingly supported by scientific evidence. While every person's nutritional needs are shaped by factors like lifestyle, genetics, health conditions, and personal preferences or values, there are a few universal pillars of a mentally nourishing diet. These include:
- Adequate protein to support neurotransmitter production and stabilise blood sugar
- Fibre to support gut health and blood sugar balance, keeping mood and energy levels steady throughout the day
- Healthy omega-3 fats to help reduce inflammation
- A wide variety of fruits and vegetables to provide essential vitamins, minerals, fibre, and antioxidants
Make sure you're getting enough sleep, make sure you're looking after your nutrition, so eating whole foods, staying away from ultra processed foods, and making sure you're getting fruit and veg every day. If you're eating good, consistent meals, then it will take away the urge to snack. Dan Tai - CrossFit athlete and Prep Kitchen ambassador
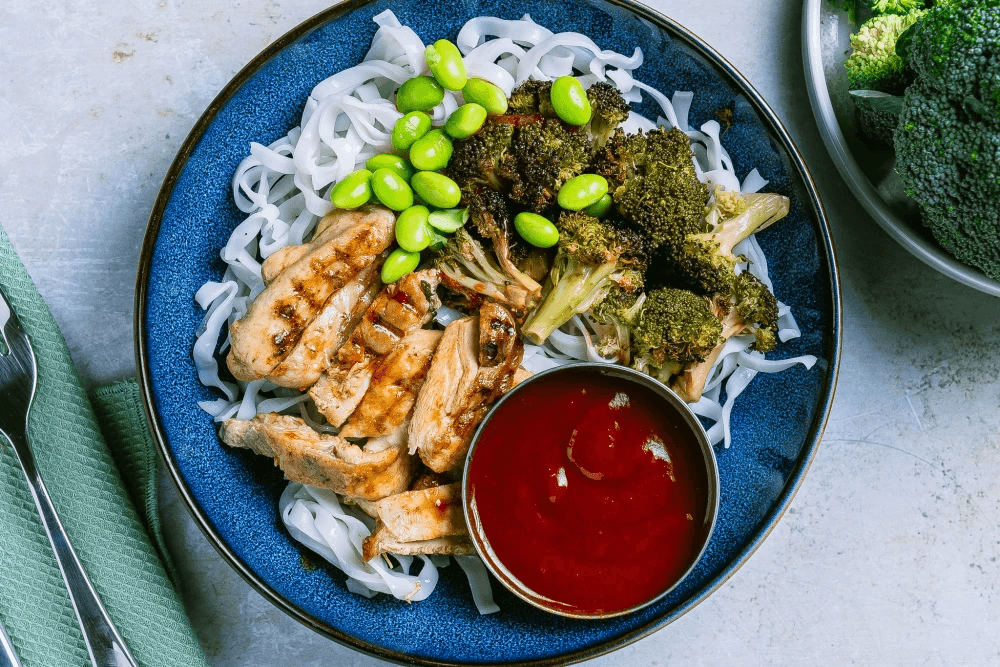
At Prep Kitchen, we're proud to offer high-protein meals with two to three portions of vegetables, designed to support mental and physical wellness. Not only that, but the time you save with a PK subscription gives you more time to practise self-care and support your wellbeing.
If you enjoyed this article, check out these other related blogs on our website:
Study Shows Meal Prep Subscription Saves Time and Money
References
Rao TS, Asha MR, Ramesh BN, Rao KS. Understanding nutrition, depression and mental illnesses. Indian J Psychiatry. 2008 Apr;50(2):77-82. doi: 10.4103/0019-5545.42391. PMID: 19742217; PMCID: PMC2738337.
Lima, M. T., Diniz, T. A., Telles, G. D., et al. (2020). The importance of protein and amino acids for mental health. Nutrients, 12(11), 3265. https://doi.org/10.3390/nu1211326
Jenkins TA, Nguyen JC, Polglaze KE, Bertrand PP. Influence of Tryptophan and Serotonin on Mood and Cognition with a Possible Role of the Gut-Brain Axis. Nutrients. 2016 Jan 20;8(1):56. doi: 10.3390/nu8010056. PMID: 26805875; PMCID: PMC4728667.
Basturk B, Koc Ozerson Z, Yuksel A. Evaluation of the Effect of Macronutrients Combination on Blood Sugar Levels in Healthy Individuals. Iran J Public Health. 2021 Feb;50(2):280-287. doi: 10.18502/ijph.v50i2.5340. PMID: 33747991; PMCID: PMC7956086.
Giuntini EB, Sarda FAH, de Menezes EW. The Effects of Soluble Dietary Fibers on Glycemic Response: An Overview and Futures Perspectives. Foods. 2022 Dec 6;11(23):3934. doi: 10.3390/foods11233934. PMID: 36496742; PMCID: PMC9736284.
Rao TS, Asha MR, Ramesh BN, Rao KS. Understanding nutrition, depression and mental illnesses. Indian J Psychiatry. 2008 Apr;50(2):77-82. doi: 10.4103/0019-5545.42391. PMID: 19742217; PMCID: PMC2738337.
Mahdavifar B, Hosseinzadeh M, Salehi-Abargouei A, Mirzaei M, Vafa M. Dietary intake of B vitamins and their association with depression, anxiety, and stress symptoms: A cross-sectional, population-based survey. J Affect Disord. 2021 Jun 1;288:92-98. doi: 10.1016/j.jad.2021.03.055. Epub 2021 Mar 26. PMID: 33848753.
Young, L. M. (2007). Folate and depression—a neglected problem. Journal of Psychiatry & Neuroscience, 32(2), 80-82.
Clemente-Suarez VJ, Redondo-Florez L, Martin-Rodriguez A, Curiel-Regueros A, Rubio-Zarapuz A, Tornero-Aguilera JF. Impact of Vegan and Vegetarian Diets on Neurological Health: A Critical Review. Nutrients. 2025 Feb 28;17(5):884. doi: 10.3390/nu17050884. PMID: 40077754; PMCID: PMC11901473.
Inflamed moods: a review of the interactions between inflammation and mood disorders. Rosenblat JD, Cha DS, Mansur RB, McIntyre RS. Prog Neuropsychopharmacol Biol Psychiatry. 2014;53:23-34. doi: 10.1016/j.pnpbp.2014.01.013. [DOI] [PubMed] [Google Scholar]
Bozzatello P, Brignolo E, De Grandi E, Bellino S. Supplementation with Omega-3 Fatty Acids in Psychiatric Disorders: A Review of Literature Data. J Clin Med. 2016 Jul 27;5(8):67. doi: 10.3390/jcm5080067. PMID: 27472373; PMCID: PMC4999787.
Guu, T. W., Mischoulon, D., Sarris, J., et al. (2019). The role of omega-3 polyunsaturated fatty acids in the treatment of depression: A review of recent literature. Current Opinion in Psychiatry, 32(1), 22-27. https://doi.org/10.1097/YCO.0000000000000462
Appleton J. The Gut-Brain Axis: Influence of Microbiota on Mood and Mental Health. Integr Med (Encinitas). 2018 Aug;17(4):28-32. PMID: 31043907; PMCID: PMC6469458.
Breit S, Kupferberg A, Rogler G, Hasler G. Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders. Front Psychiatry. 2018 Mar 13;9:44. doi: 10.3389/fpsyt.2018.00044. PMID: 29593576; PMCID: PMC5859128.
Konstantinidis T, Tsigalou C, Karvelas A, Stavropoulou E, Voidarou C, Bezirtzoglou E. Effects of Antibiotics upon the Gut Microbiome: A Review of the Literature. Biomedicines. 2020 Nov 16;8(11):502. doi: 10.3390/biomedicines8110502. PMID: 33207631; PMCID: PMC7696078.
Tetel MJ, de Vries GJ, Melcangi RC, Panzica G, O'Mahony SM. Steroids, stress and the gut microbiome-brain axis. J Neuroendocrinol. 2018 Feb;30(2):10.1111/jne.12548. doi: 10.1111/jne.12548. PMID: 29024170; PMCID: PMC6314837.
Antinozzi M, Giffi M, Sini N, Galle F, Valeriani F, De Vito C, Liguori G, Romano Spica V, Cattaruzza MS. Cigarette Smoking and Human Gut Microbiota in Healthy Adults: A Systematic Review. Biomedicines. 2022 Feb 21;10(2):510. doi: 10.3390/biomedicines10020510. PMID: 35203720; PMCID: PMC8962244.
Nagpal R, Shively CA, Register TC, Craft S, Yadav H. Gut microbiome-Mediterranean diet interactions in improving host health. F1000Res. 2019 May 21;8:699. doi: 10.12688/f1000research.18992.1. PMID: 32704349; PMCID: PMC7359750.
Lane M M, Gamage E, Du S, Ashtree D N, McGuinness A J, Gauci S et al. Ultra-processed food exposure and adverse health outcomes: umbrella review of epidemiological meta-analyses BMJ 2024; 384 :e077310 doi:10.1136/bmj-2023-077310
Lassale C, Batty GD, Baghdadli A, Jacka F, Sanchez-Villegas A, Kivimaki M, Akbaraly T. Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol Psychiatry. 2019 Jul;24(7):965-986. doi: 10.1038/s41380-018-0237-8. Epub 2018 Sep 26. Erratum in: Mol Psychiatry. 2019 Jul;24(7):1094. doi: 10.1038/s41380-018-0299-7. Erratum in: Mol Psychiatry. 2021 Jul;26(7):3657. doi: 10.1038/s41380-021-01056-7. PMID: 30254236; PMCID: PMC6755986.
Suhag K, Rauniyar S. Social Media Effects Regarding Eating Disorders and Body Image in Young Adolescents. Cureus. 2024 Apr 21;16(4):e58674. doi: 10.7759/cureus.58674. PMID: 38770510; PMCID: PMC11103119.